Sleep. It’s a natural process that you shouldn’t have to think about, fret about, or deal with. Every animal sleeps, after all. But for you, sleep isn’t easy. Whether you suffer from insomnia or sleep apnea, a lack of consistent, restful sleep can take a serious toll on relationships, performance, mood, and cognition. Poor sleep affects your every waking moment. Fortunately, sleep doctors can help.
As a Sacramento dentist who has studied sleep medicine for years, Dr. Timothy Mickiewicz is well acquainted with the negative effects sleep deprivation has on the human body. Dr. Mick helps patients with the most common form of sleep apnea, obstructive sleep apnea, to find solid, consistent rest so that they live productive, positive lives. Don’t let poor sleep dictate how you think, act, and live. Call Dr. Mickiewicz for a consultation now.
In today’s blog, you’ll learn:
- About healthy sleep cycles
- The most common sleep disorders
- Statistics about sleep quality in America
- How sleep studies work
- What obstructive sleep apnea is
- Treatment for sleep apnea
A Healthy Sleep Cycle
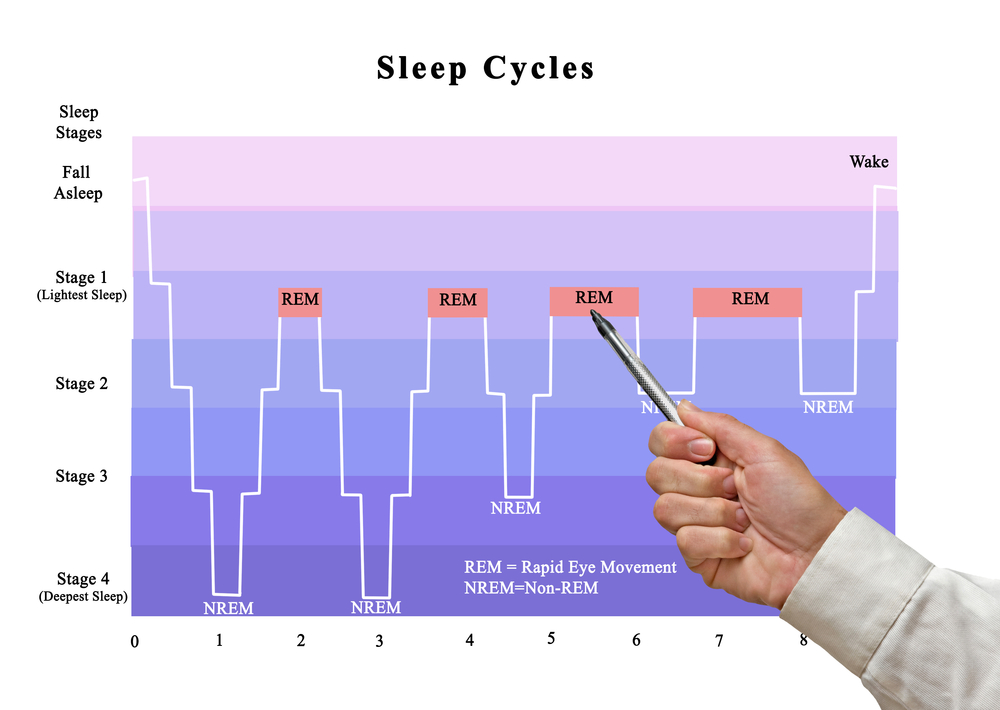
By assessing brain activity and rapid eye movement during sleep, sleep doctors have learned that human sleep happens in cycles. On average, a person has four to six cycles that begin every 80 to 100 minutes. Between sleep cycles, we may wake, but only briefly.
Sleep doctors will tell you that humans have two primary phases of sleep. REM stands for rapid eye movement, the phase that involves high brain activity and eyes twitching behind closed lids. Most of our dreaming occurs during REM sleep when muscles are lax so that sleepwalking doesn’t occur.
As the night progresses, we accomplish more REM sleep. Interestingly, we have less REM sleep when we’re cold because the body doesn’t regulate its temperature well during REM.
The other phase of sleep is non-REM sleep, and it involves three stages:
- The transition between wake and sleep
- Sleep
- Deep, or slow-wave, sleep (occurs earlier in the night)
When we’re born, most of our sleep is REM. As we grow to become children, the time we spend in non-REM deep sleep increases. Then, in our teen years, deep sleep shortens and continues to do so throughout life. Elderly people may never reach deep sleep.
What is circadian rhythm?
You may have heard the term “circadian rhythm.” This refers to a 24-hour cycle of behavioral, mental, and physical changes that occur as the body responds to light and dark. All living things, from plants to animals to microbes, are affected by circadian rhythms. The rhythms impact the release of hormones, body temperature, digestion, and eating habits in humans.
How much sleep do sleep doctors recommend for the average adult?
The National Sleep Foundation tells us that adults should sleep seven to nine hours per night, but 30% of us achieve less than six hours per night. Thirty-five percent of Americans get poor or fair sleep.
The Most Common Issues Treated by Sleep Doctors
Also called sleep-wake disorders, sleep disorders disturb the amount of sleep a person achieves, as well as sleep quality and timing. Approximately 50 million people in the US suffer from chronic (long-term) sleep disorders.
Insufficient sleep leads to sleep deprivation, which causes a list of health concerns and risks, in addition to poor energy, depression, and slow reaction times. Accidents increase when a person suffers from sleep deprivation. Children who sleep poorly may suffer from poor growth and development, as well as problems with learning and school.
Generally, poor sleep increases the risk for:
- Stroke
- High blood pressure
- Coronary heart disease
- Obesity
Insomnia is the number-one sleep disorder, followed by snoring and obstructive sleep apnea. Insomnia is defined as difficulty falling or staying asleep. Some people have short bouts of insomnia, but insomnia disorder occurs when a person suffers from insomnia three or more nights a week, for a period longer than three months. These patients often experience the effects of sleep deprivation. Over 40% of insomniacs suffer from a mental disorder, as well.
The second most prevalent sleep disorder is sleep apnea, which involves apneic episodes when a person stops breathing for 10 seconds to a minute or more, repeatedly throughout the night. The prevalence of sleep apnea is higher in older populations, and in males more than women. We will examine sleep apnea in more detail later in this article.
Sleep Study Options
Sleep doctors use sleep studies to diagnose and treat sleep disorders. In most cases, patients stay overnight in a sleep lab, while polysomnography monitors: eye movement, brain activity, blood-oxygen levels, and leg movements.
Alternatively, Dr. Mickiewics offers a home sleep study.
In the comfort and familiarity of your own bed, a home sleep study is often preferable to an overnight sleep study in a lab. For the home sleep study, you’ll be given a sleep study unit, with instructions on how to wear the monitor(s) so that it records data about your sleep.
Sleep study results are interpreted by a sleep doctor, who diagnoses sleep disorders. From there, you’ll be advised of treatment options to help alleviate your sleep disorder, so you can enjoy an improved quality of life.
3 Types of Sleep Apnea
If you are diagnosed with sleep apnea, it will be one of three types:
- Obstructive sleep apnea – the most common type; soft tissues in the mouth and throat collapse during sleep to cause apneic episodes
- Central sleep apnea – has do to with the brain not communicating properly with muscles that control breathing
- Complex sleep apnea – a combination of obstructive and central sleep apnea
Obstructive Sleep Apnea
As the most common form of sleep apnea, obstructive sleep apnea (OSA) occurs when soft tissues of the mouth and throat block airflow. At first, a patient may snore loudly as the soft tissues vibrate upon inhaling and exhaling. Ultimately, those soft tissues disrupt breathing. The resulting apneic episodes can happen many times during the night, for a duration of ten seconds to well over 60 seconds.
Patients may awake suddenly while choking or gasping. This is the body’s response to low blood oxygen; it tries desparately to inhale. The patient wakes enough to resume normal breathing until soft tissues again block airflow and another apneic episode occurs.
Without treatment, OSA patients may experience:
- Loud, chronic snoring
- Morning headaches or migraines
- Dry mouth or sore throat upon waking
- Daytime drowsiness or fatigue
- Falling asleep at times of low stimulation
- Poor performance at work/school
- Cognitive issues
- Poor focus
- Memory issues
- Higher incidence of accidents
- Depression/moodiness
- Decreased sex drive/impotence
Additionally, people who sleep within earshot of a loud snorer may also experience poor sleep and sleep deprivation. Obstructive sleep apnea can place a strain on a relationship when neither partner sleeps well.
Treatment for OSA
If you’ve been diagnosed with OSA and cannot tolerate wearing a CPAP every night, or you suspect that you suffer from a sleep disorder, call Dr. Mickiewicz. For years, Dr. Mick has helped OSA patients achieve healthy sleep by wearing a sleep guard. This oral appliance keeps the lower jaw slightly forward, but in a comfortable position that allows breathing to remain unphased throughout sleep. As a bonus, loud snoring also stops when a patient wears a sleep guard.
Schedule your consultation with sleep doctor Dr. Timothy Mickiewicz in Sacramento by calling 916.469.9178.