 Are we going too far?
Are we going too far?
For millennia, doctors have battled to discover the cause of pain: a nebulous and subjective complaint, called by some the “fifth vital sign,” included after temperature, blood pressure, pulse and respiration. How can we measure this with any accuracy? Certainly, those of us in the pain trenches are faced many times per day with the dilemma of how to objectify a subjective symptom. Are visual analog scales and goofy schematics adequate?
I have no doubt that pain is real, and dentists love to measure things, preferably in microns. But we can’t put a pain patient in our standard differential box. I have no doubt the pain is real because, frankly, I live it every day; I am shocked at the number of referrals that I see writhing and crying—face furrowed, verbalization difficult—yet no previous doctor has tried a simple nerve block. The patient presents with diffuse jaw pain, x-rays negative, pulp test negative, multiple root canal therapies to no avail—yet the simple act of numbing up the area is such a forgotten technique. Why, Doc? If the pain goes away, great, now focus on the etiology. If it does not, you have a real problem on your hands.
Integrative Pain Management, SSRIs, and Functional Medicine
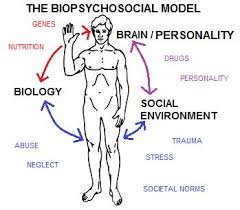
I was a founding member of the American Academy of Pain Management, and earned Diplomate status. I went through an exhaustive credentialing program resulting in the accreditation of my pain program, which was unprecedented for a non-university-based program. Now, 26 years later, they are the Academy of Integrative Pain Management! This renaming shows a clear paradigm shift in the role of looking beyond organic etiology and looking to the mind/body/spirit as the origin of pain.
So how do we approach this poor patient writhing in pain? First, we listen.
Listening is your best diagnostic tool, and it may be the only one you need. Too often, we are so caught up in the obvious that we miss the glaring signs of heightened stress level, and physical or mental abuse—compounded by the frustration that five other doctors never really took the time to listen before the prescription pad came out.
Thankfully, we are now paying more attention to overuse of opioids, but without this crutch the tough part begins. Unfortunately, the average physician is lucky to get 15 minutes with a patient to figure out what’s going on, so frequently it’s SSRIs to the rescue—or a dedicated pain doctor to sort out the mess.
This whole blog is purposely as disjointed and complicated as the patient in front of you. All over the board, with complicated and thought-provoking statements. Why? Because this endeavor is not for everyone. The empathy and compassion necessary to understand your patient is not the same as drilling and filling. You can’t just squeeze them in between the crown prep and the hygiene check. Sometimes you have to dedicate an hour to really review the case, face to face.
Do we forgo our basic training and not look at the organic etiology? Tragically, I think this is the trend in the industry. Venerated institutions like the Cleveland Clinic are establishing “functional medicine,” integrating so many forms of alternative treatment modalities, it is hard to track. Who am I to call them out on their approach? Just one doc in the battle, faced with a procession of patients who, for the past 30 years, do get better after they see me (based on our outtake forms, at least).
A Way Forward
My secret is having open ears to listen and an open mind to the alternative, never forgetting my evidence-based science. Couple that with an understanding of trigger point injection and nerve blocks, having a team of physicians to call on and refer to, and you are a safe beginner in the world of pain management.
A weekend course is not enough. But we need you: someone to join the battle. There are plenty of challenges to go around and many patients who, tragically, have just given up. As we continue this exposure, dig deep to see if you want to spend your Saturday night reading medical journals and browsing PubMed for information. Please do. The rewards are priceless.
About the Author: Dr. Mickiewicz owns a private practice in Sacramento and lectures across the nation on TMD treatments. He is a diplomate of the American Academy of Pain Management and holds membership in many professional associations for dentistry, sleep medicine, and TMD. In addition, Dr. Mick, as his patients call him, founded Pacific Orofacial Pain Consultants, a team of experts in various disciplines, who tackle the issue of TMD pain and treatment, to help sufferers find relief from chronic pain. To talk with Dr. Mick, call his Sacramento dental office at 916-457-7710.